Health
Diabetes as a development issue
[ By David Whiting ]
Diabetes is a chronic, non-communicable disease. There are two main types: type 1 is diagnosed primarily in the young and is characterised by the absence of insulin; type 2 is usually diagnosed in adults and is characterised by a relative insufficiency of insulin. Both forms of diabetes lead to serious complications if not managed properly – including damage to sight and nerves, kidney disease, amputations and increased risk of cardiovascular disease, such as strokes, for example.
The causes of type 1 are largely unknown, although there is some evidence of a link to infections. The causes of type 2 diabetes are largely related to economic development. Urbanisation, mechanisation and globalisation lead to reduced physical activity and a diet that contains more fat and salt, which in turn lead to obesity and raised blood pressure. Diabetes therefore is a development issue.
According to the International Diabetes Federation, currently 246 million people worldwide live with diabetes and it is expected that 380 million will be affected by 2025. This will mostly concern people aged 45-64 years in low- and middle-income countries. So by 2030 more than 80 % of people with diabetes will live in what is currently called a “developing country”.
Diabetes is also a major cause of death. In the year 2000 diabetes caused the deaths of three million people – as many as died from HIV/AIDS in the same year. Besides causing premature death, diabetes also leads to “complications”. This understated medical term trivializes the results of poorly controlled diabetes. When blood glucose and blood pressure levels are too high for too long they cause damage to blood vessels and nerves. Damage to large blood vessels results in increased risk of heart disease and stroke. Damage to small blood vessels of the eye causes diabetes retinopathy, the leading cause of blindness in industrialised countries. Damage to the kidneys (nephropathy) is the leading single cause of end-stage renal disease in the USA and Europe, accounting for 40 % of new cases in the USA. People with end-stage renal disease require either dialysis or a kidney transplant – both being rarely available in low-income settings.
Damage to sensory, motor and autonomic nerves – neuropathy – can result in a variety of symptoms, including loss of sensation, tingling and pain, muscle atrophy, loss of muscle control, increased sweating, digestion, heart rate and blood pressure. Damage to nerves and blood flow put people with diabetes at risk of foot ulcers. A small cut or bruise can go unnoticed and fail to heal. If allowed to progress these can rapidly develop into deep wounds and get septic, becoming very difficult to heal – and may finally result in amputation. In low-income countries, such as Tanzania, foot ulcers are an important cause of hospital admissions and death in people with diabetes.
Low life expectancy
People with type 1 diabetes need daily injections of insulin to survive. In poor regions– and thus in most African countries – insulin supplies are erratic, even in the largest hospitals. At current prices few can afford to buy insulin privately. The life expectancy of a child in Africa diagnosed with type 1 diabetes can be as low as one year in rural areas and eight years in urban Mali.
There is now good evidence of a general association between socio-economic position and health, with a gradient seen in a number of conditions. This gradient is also present in the factors that lead to type 2 diabetes, in outcomes for people with diabetes and in its consequences.
In the rich countries people of lower socio-economic position are less likely to engage in regular physical activity, and more likely to eat a diet that is high in salt and fat and low in fibre, and they also are more likely to smoke. The reasons behind these associations can be complex and are not fully-understood, but one important factor is the fact that high-fat poor-quality food is cheaper than healthier alternatives.
There is also evidence that conditions during pregnancy affect the risk of diabetes later in life, with poor nutritional conditions during pregnancy 'pre-programming' the foetus to be prepared for life in a constrained environment. If children born with low birth-weight grow up in an environment with an abundant supply of high-energy food and are less physically active, they are at an increased risk of diabetes. This is particularly important for children of people who migrate from low- to high-income countries, or from rural to urban communities.
As low-income countries develop, those in the higher socio-economic groups are at increased risk initially. This situation is soon reversed however and even in places such as urban Tanzania the prevalence follows a gradient with the proportion of those of lower socio-economic position having diabetes being larger.
Social injustices
There are also inequalities in diabetes outcomes, and these are stronger in countries that do not have universal health care. In countries such as the USA, people without health insurance have less frequent examinations and worse outcomes – more eye disease, for example. In countries that have universal health care that is free at the point of access, income-related measures of socio-economic position are less strongly associated with control. Many low-income countries have engaged in reforms of the health sector in the last decade and some have introduced cost-sharing, which may lead to inequalities. Health care for diabetes in some African countries is very limited, and tends to be concentrated in urban centres and secondary health facilities, limiting access to care.
The consequences of type 1 diabetes have been studied much more than those of type 2. Poor control and the presence of complications are associated with lower quality of life and with more depression – these states are more likely in people of lower socio-economic position.
One of the few studies that explicitly examines inequalities in expenditure comes from India. This nationally representative study in urban and rural India found that there was a gradient in the proportion of income spent on diabetes care, with those in the lower socio-economic groups spending a larger proportion of their income on diabetes care than those in the higher groups in both urban and rural areas.
Economic impact
Diabetes is also an important development issue because it has a large economic impact. In higher-income countries more than half of those with diabetes are older than 65 years. In countries from the south most people affected are aged 45-64 years, and are thus of economically-productive age. Therefore the individual losses resulting from complications and premature mortality are also economic losses for low-income countries. And these are likely to undermine the MDGs.
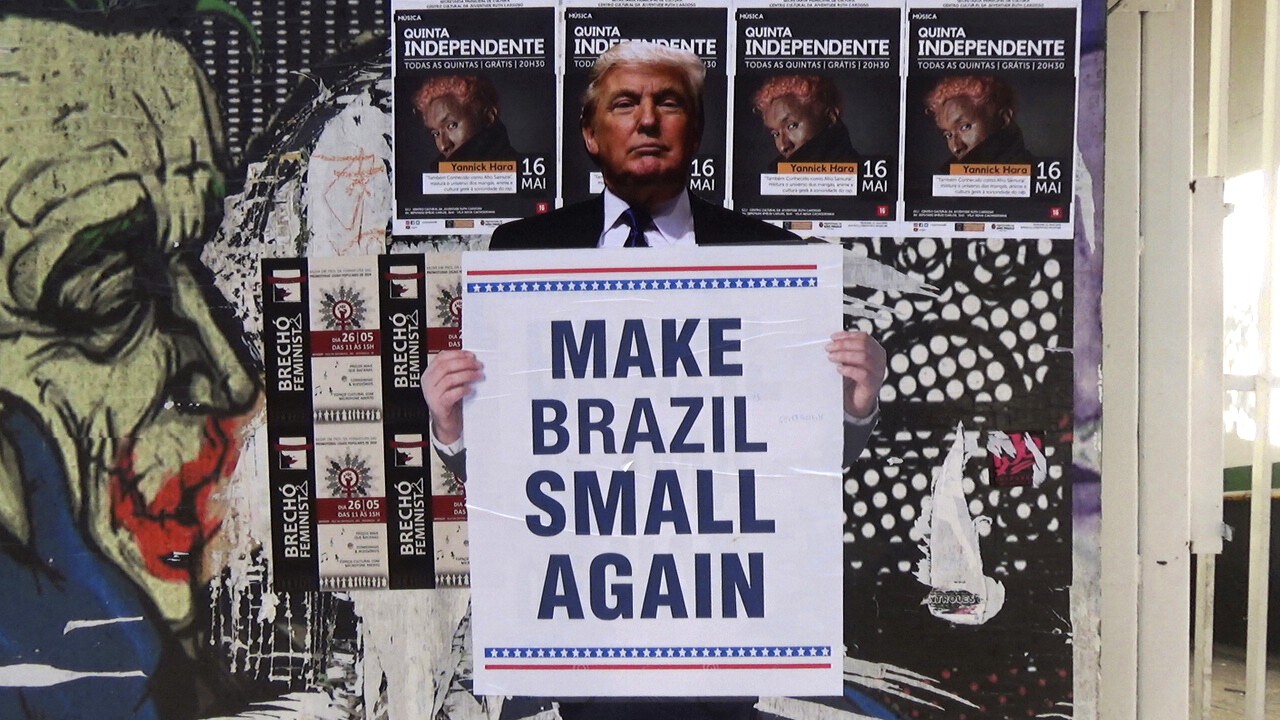
Considering mainly the effects of premature mortality, the World Health Organization (WHO) estimates that between 2005 and 2014 diabetes, heart disease and stroke combined will cost $555.7 billion in lost national income in China, $336.6 billion in India, $49.2 billion in Brazil and $2.5 billion even in a poor country like Tanzania. Much of the heart disease and stroke in these estimates is linked to diabetes.
80 % of expenditure on care for diabetes is in a handful of higher-income countries – meanwhile 80 % of people with diabetes will soon be living in developing countries. Half of the $232 billion that is estimated to have been spent on diabetes care in 2007 was spent in the USA, another quarter ($64 billion) in Europe. At the other extreme, India, the country with the largest number of people with diabetes in the world, spent 0.9 %. All African countries combined spent just 0.3 % of the global total.
In most western countries a good portion of money on diabetes is spent via the health system, whereas in poor countries out-of-pocket expenses can be considerable. For example, in Latin America families pay 40-60 % of expenditures for medical care from their own pockets and in some of the poorest countries families bear almost the entire cost of care.
Governmental action needed
Urbanisation and development have led to improvements in health and quality of life. As poor countries develop, efforts need to be made to ensure that development is healthy and sustainable. These countries have the opportunity to learn from the mistakes already made in countries that have more established urban communities – for example to plan the development of cities that facilitate and encourage physical activity and promote healthy eating. By planning appropriately the predicted increases in the number of people with diabetes in developing countries might be avoided. If, however, the prediction happens to become reality, the premature mortality, reduced quality of life, loss of economic production and increased health care costs will be a terrible additional burden for people in low-income countries to bear.