Health
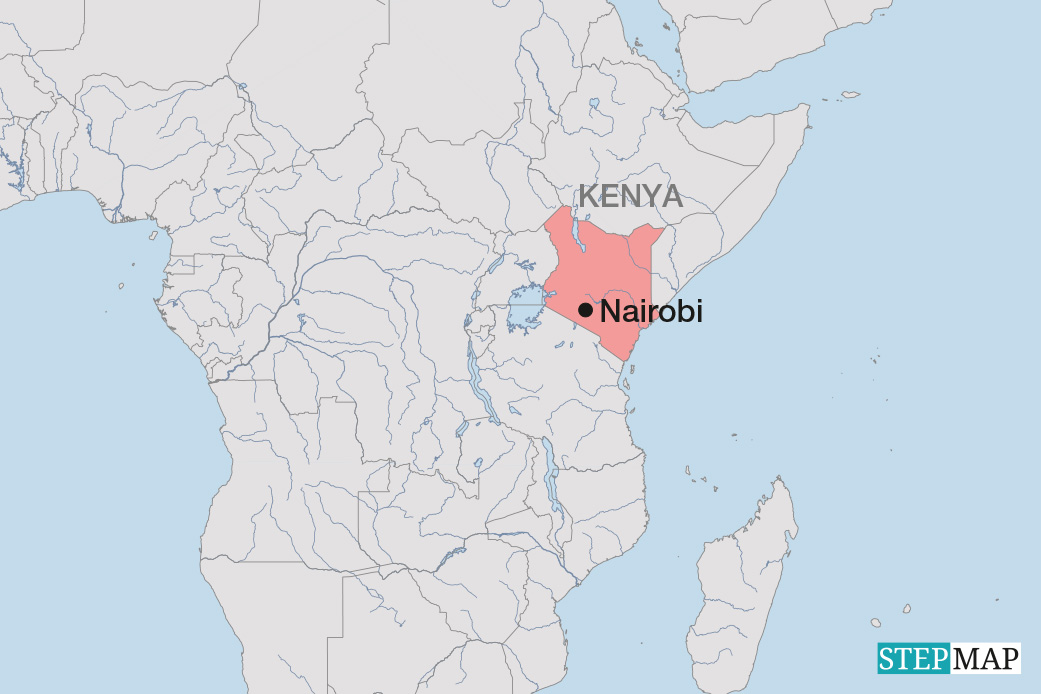
Systemic failure

In Syria, in October 2013, the first new cases of polio were registered. The disease had not occurred in the country for years, but because of the civil war, more than half a million children were not vaccinated. The World Health Organisation (WHO) and the UN children’s agency UNICEF are now preparing the biggest vaccination campaign they have ever mounted. They plan to inoculate as many as 20 million children across the region to prevent the resurgence of a disease that was nearly eradicated.
In Greece, in the summer of 2012, the first cases of domestic malaria were noticed in decades. In the course of the Euro crisis, the government had slashed its health-care budget and discontinued insect control programmes. Moreover, HIV infection doubled because of massive reductions in syringe exchange programmes for drug users (Stuckler 2013).
In Russia, India and South Africa, tuberculosis (TB) is becoming increasingly difficult to treat. Doctors are encountering more and more multi-resistant and ultra-resistant forms of TB, which can only be treated with extremely complex, lengthy and costly courses of drugs with lots of side effects. The trend has been confirmed for all three countries in the WHO’s Global Tuberculosis Report.
These cases are very different, but they have one thing in common: disease is increasing because of inadequate or unavailable health care. Since people typically blame the spread of diseases on viruses and bacteria, it is important to point out that health-care systems are at the root of the problem too. That can be blatantly obvious, as in the case of Syria for example.
Syria’s public health-care system has collapsed in many parts of the country. Millions of people have fled from conflict areas, and neither the Syrian Red Crescent, which is close to the government, nor the humanitarian aid, that the rebels get, can take care of displaced persons. So for three years, routine infant vaccinations have simply not been performed.
In the case of Greece, the health-care disaster was not caused by a war, but by massive budget cuts. The Greek government has been tightening its budget as a consequence of its bail-out agreements with the country’s main creditors. It is implementing the austerity policy favoured by the European Central Bank, the European Commission and the International Monetary Fund.
In the past few years, most reports of the Greek health crisis have told of acutely ill patients who lost their health-insurance protection along with their jobs and faced high charges for hospital admission in emergencies or large bills for medication. As cuts in key preventive programmes such as mosquito control or syringe-exchange schemes had no immediate impact, they got little media attention. Today, however, it is obvious that disease prevalence is rising.
In regard to TB in India, Russia and South Africa, the trouble stems from home-made problems in the health-care system. Poor or marginalised patients, in particular, get insufficient support. They face inflexible institutions and/or high costs. The problem is not the medication, which most TB programmes provide free of charge. Major hurdles include the costs of travelling to a treatment centre or the loss of time and income. These are huge challenges for people who work in the informal sector. Many of them fail to complete the months-long course of treatment that is necessary to really cure TB.
Such failure puts the patient concerned at risk of the disease flaring up again. There is another danger however. Discontinued treatment promotes the development of bacteria that are resistant to standard TB drugs. This is a public issue – and it concerns other nations too.It is true that TB patients no longer need to spend months in hospital. Outpatient support has become feasible. Nevertheless, the length of treatment still remains a major challenge. To the extent that health-care systems do not rise to this challenge, TB is becoming more dangerous again.
International responsibility
My examples illustrate why experts all over the world are beginning to reconsider health-care systems. For years, professionals at the WHO and elsewhere focused chiefly on the control of major diseases. They dealt with HIV/AIDS, TB and malaria as well as global influenza epidemics. They also took interest in “new epidemics” of chronic, non-infectious cardiovascular, respiratory and metabolic diseases. But controlling specific diseases is not enough. To provide global protection from epidemics and serious illnesses, it is important that local health-care systems work. Otherwise, disease will only spread faster. Health is thus a global public good, and providing health care a global responsibility.
The latest buzzword is “universal health coverage” (UHC). Headlined by the WHO in its World Health Report 2010, UHC has become one of the most widely discussed terms in expert circles. In the debate on the post-2015 global development agenda, in particular, it has become very popular.
It is no coincidence, of course, that the word “coverage” was taken from the insurance industry. For years, the “catastrophic health-care costs” that poor people and even members of the rising middle classes face in the increasingly privatised health-care systems of the developing world have been a central topic in every speech made by the WHO’s director-general. According to estimates, some 100 million people drop into poverty every year. Many of the very poor do not benefit from health-care services at all because they cannot afford the charges levied by health centres and hospitals. Bribes demanded by often underpaid health-professionals are a related problem that typically haunts under-funded public health-care systems.
Accordingly, the WHO defined UHC as people having safe access to health-care services, regardless of whether they can pay or not. They should be protected from exorbitant costs. The keywords are availability, accessibility and affordability.
However, that definition of UHC soon came under heavy fire. Critics from civil society say it focuses too much on the economic accessibility of health-care services. They also warn that this concept may lead to private health-care providers developing new finance models and reaching target groups beyond the affluent upper classes, in which case public health care would degenerate into a meagre default system for poor people.
That is precisely what Brazil is currently experiencing. The country’s Universal Health System formally offers a comprehensive health-care service for every citizen. However, private-sector providers are attracting the better-off with additional benefits and better service, leaving the public sector to shoulder the burden of huge, but unprofitable health risks.
Most countries have some kind of multi-class system in health care. Accordingly, it would be wrong for the post-2015 development goals to be geared exclusively to funding. Civil-society activists fear that a concept that sounds progressive will be trimmed down in view of limited resources, so it will ultimately only offer minimal coverage for the poor in many countries, unless those patients pay for additional care out of their own pockets.
Experts also criticise the WHO’s narrow focus on the health sector. Its UHC concept only takes into account issues such as information, awareness raising, prevention, treatment and rehabilitation, and it neglects the social determinants of health. In the late 1970s, the WHO’s Primary Health Care Concept had also tackled issues such as education, income, housing, food security and social inclusion. In comparison, the UHC focus on the prevention and cure of illness reflects a truncated understanding of health. It is good, however, that sufficient and adequately-paid professionals have been acknowledged as indispensable for appropriate health care in recent WHO documents. Social determinants have also been mentioned once more.
More health or more medicine?
The importance of health-care quality – and not just accessibility and availability – is evident in Indian and Bangladeshi programmes to reduce maternal mortality, a Millennium Development Goal. Attempts were made to reduce the number of home deliveries in favour of deliveries in hospitals. But it turned out that the quality of institutional obstetrics was often inadequate, so the risks for pregnant women were sometimes even greater than under the supervision of traditional midwives. In these settings, focussing on midwives is the right approach.
To make sure that “more health” is not equated with “more medicine”, monitoring is essential. It is a well-known fact that all health-care systems – and especially private providers – tend to develop services of questionable value and then market those services. UHC must be embedded in a human rights framework. The International Covenant on Economic, Social and Cultural Rights, which was adopted by the United Nations in 1966, set the right example. It spelled out a “right of non-discriminatory access to health-care services” and included the social determinants of health. Furthermore, it must be stressed that people deserve a say in major health-relevant decisions at the national and international levels.
Unfortunately, the WHO’s UHC concept does not include these things to date. As a result, international debate is focussing too narrowly on financing. It is not enough to only discuss what service packages can be funded, what minimum-protection levels should be and what shares of spending should be afforded by the public and private sectors.
Humanity needs a debate on global solidarity, not just funding. Global solidarity is needed to make good health care for everyone come true. Even if low-income countries managed to raise more taxes and made optimal use of their budgets, many of them would hardly be in a position to fund more than rudimentary health care for all their people.
There is more at stake than each country to finance its own health-care system. We must rise to a global responsibility. Mandatory financing mechanisms are required at the international level, and the global economy needs to be redesigned for greater social sustainability (Labonté 2007). If this is taken into account, the post-2015 development goals will not only apply to the countries of the global South – they will become truly global issues that concern everyone.
References:
Stuckler, D., and Basu, S., 2013: The body economic. Why austerity kills. Recessions, budget battles, and the politics of life and death, p.77–94.
Labonté, R., and Schrecker, T., 2007: Globalisation Knowledge Network: Towards health-equitable globalisation. Rights, regulation and redistribution. Final report to the Commission on Social Determinants for Health, 2007, p. 116–130.
http//www.who.int/social_determainants/resources/gkn_reports_06_2007.pdf